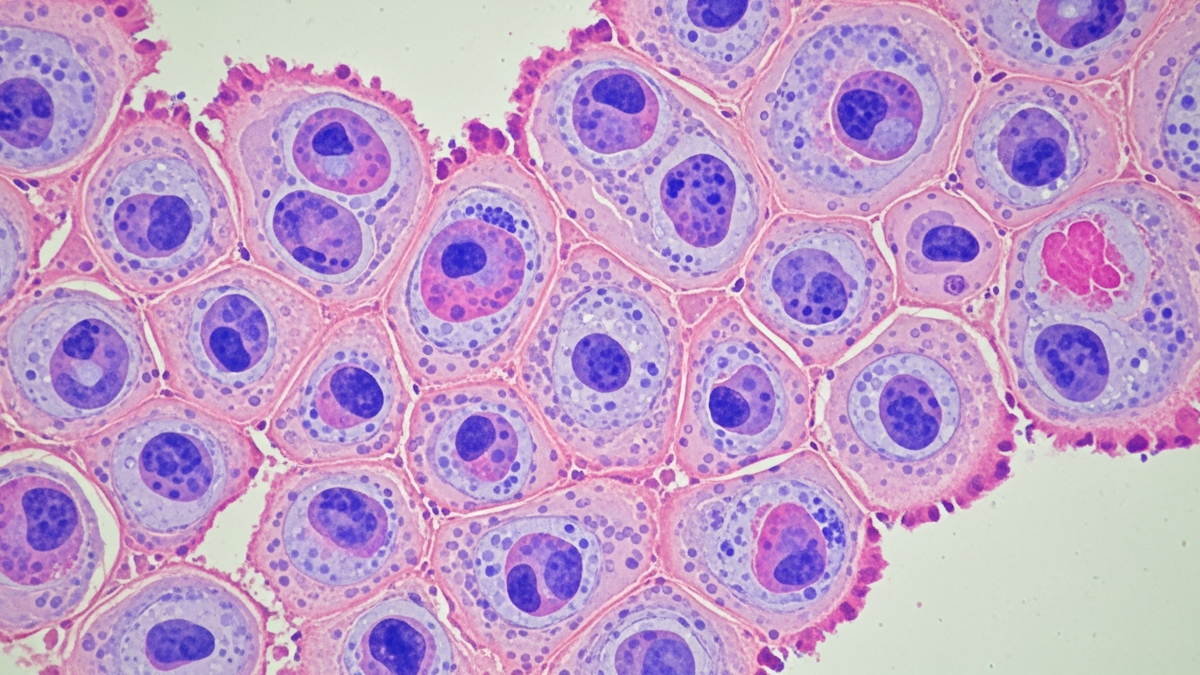
Pfizer Inc. and Astellas Pharma Inc. have announced that the U.S. Food and Drug Administration (FDA) has approved PADCEV (enfortumab vedotin-ejfv), a Nectin-4 directed antibody-drug conjugate (ADC), in combination with the PD-1 inhibitor Keytruda (pembrolizumab) or Keytruda QLEX (pembrolizumab and berahyaluronidase alfa-pmph), as neoadjuvant treatment and then continued after cystectomy (surgery) as adjuvant treatment for adult patients with muscle-invasive bladder cancer (MIBC) who are ineligible for cisplatin-containing chemotherapy.
The approval of this perioperative (before and after surgery) treatment was based on results from the pivotal phase 3 EV-303 clinical trial (also known as KEYNOTE-905), which were presented during a Presidential Symposium at the European Society of Medical Oncology (ESMO) Congress 2025.
Matthew Galsky, Lillian and Howard Stratton Professor of Medicine, director of Genitourinary Medical Oncology, Mount Sinai Tisch Cancer Center, and EV-303 investigator, said: “Enfortumab vedotin plus pembrolizumab is poised to address a critical unmet need. Half of patients with MIBC may experience cancer recurrence even after having their bladder removed, and many of these patients are ineligible to receive cisplatin. This approval, based on striking event-free and overall survival benefits, may represent an important practice-changing advance for these patients who’ve had no new options in decades.”
Jeff Legos, chief oncology officer at Pfizer, said: “Today’s approval, granted months earlier than anticipated, ushers in a new era of treatment for cisplatin-ineligible patients with MIBC who have long been underserved by existing treatments. PADCEV plus pembrolizumab is the first and only FDA-approved perioperative treatment regimen to demonstrate a meaningful survival advantage compared to surgery alone, positioning it to reshape the treatment landscape and bring new hope to patients and families.”
In the EV-303 study, perioperative treatment with PADCEV plus pembrolizumab resulted in a 60% reduction in the risk of tumour recurrence, progression or death compared to surgery alone, meeting the primary endpoint of event-free survival (EFS). The probability of remaining event free was 74.7% for patients who received the combination and 39.4% for patients treated with surgery only. The estimated median EFS has not yet been reached for the combination arm versus 15.7 months for the surgery arm. Data from the key secondary endpoint of overall survival (OS) showed that perioperative treatment with PADCEV plus pembrolizumab also resulted in a 50% reduction in the risk of death as compared to surgery alone. The probability of survival at two years was 79.7% for patients who received the combination relative to 63.1% for patients treated with surgery only. The estimated median OS has not yet been reached for the combination arm versus 41.7 months for the surgery arm.
Moitreyee Chatterjee-Kishore, head of oncology development at Astellas, said: “Building on the combination’s established role in locally advanced or metastatic urothelial cancer where it is has become standard of care in the US, PADCEV plus pembrolizumab now has the potential to redefine care in an earlier disease setting as the only antibody-drug conjugate and PD-1 inhibitor regimen for cisplatin-ineligible patients with MIBC. The approval underscores our unwavering commitment to expanding the reach of this innovative combination to more eligible patients with bladder cancer.”
The safety results in EV-303 were consistent with those previously reported for this combination, and there were no new safety signals. The most common (≥20%) adverse reactions, including laboratory abnormalities, in patients treated with PADCEV plus intravenous pembrolizumab were increased glucose, decreased hemoglobin, increased aspartate aminotransferase, rash, increased alanine aminotransferase, fatigue, pruritus, increased creatinine, decreased sodium, decreased lymphocytes, peripheral neuropathy, increased potassium, alopecia, dysgeusia, diarrhoea, decreased appetite, constipation, nausea, decreased phosphate, urinary tract infection, dry eye, and decreased weight. Grade ≥ 3 AEs due to any cause occurred in 71.3% of patients treated in the combination arm and 45.9% of patients who were in the surgery arm.