A research team led by Eijiro Miyako at the Graduate School of Advanced Science and Technology, Japan Advanced Institute of Science and Technology (JAIST), has discovered that the marine bacterium Photobacterium angustum demonstrates remarkable therapeutic efficacy against colorectal cancer.
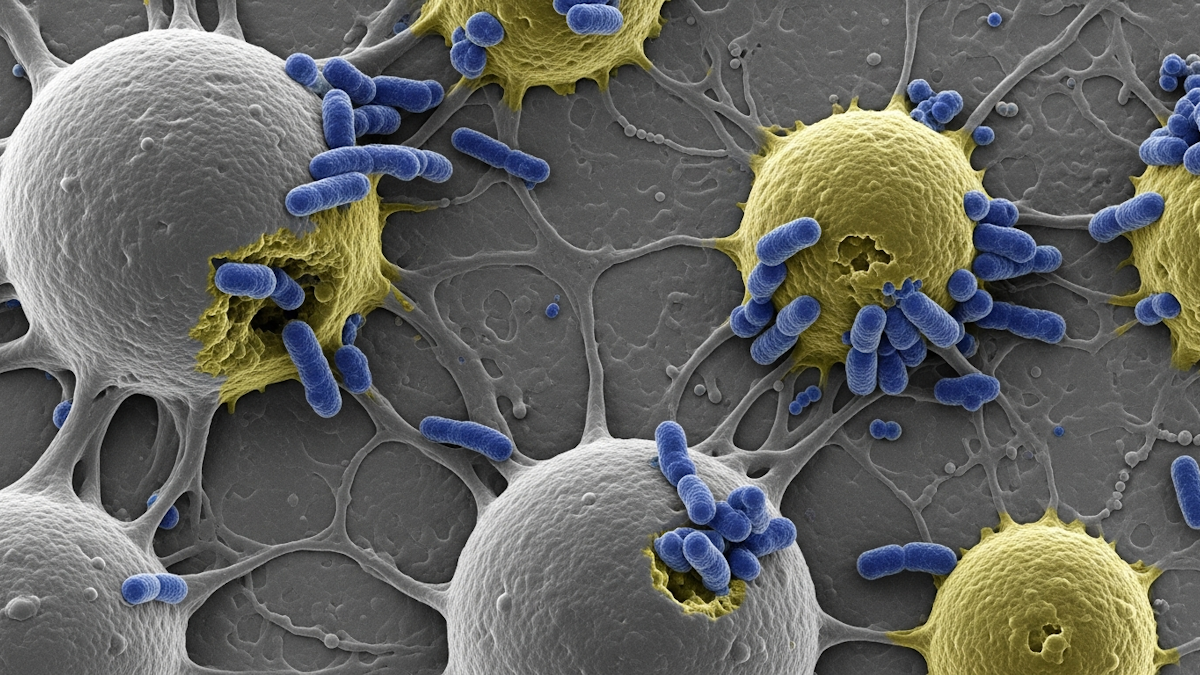
Through screening of multiple marine bacterial strains, the researchers found that P. angustum, in its natural, non-engineered form, selectively accumulates in tumour tissues and induces both direct tumour lysis and robust immune activation. In mouse models, intravenously administered P. angustum showed high tumour tropism while exhibiting minimal colonisation of vital organs except the liver, with no haematological abnormalities or histological toxicity observed.
P. angustum therapy promoted intratumoral infiltration of immune cells including T cells, B cells, and neutrophils, and enhanced production of inflammatory cytokines such as tumour necrosis factor-α (TNF-α) and interferon-γ (IFN-γ). The bacterium also demonstrated intrinsic oncolytic activity through natural exotoxin production, directly destroying cancer cells. These combined mechanisms significantly prolonged survival in treated mice, with complete remission achieved in some cases.
This research represents a critical advance toward developing safer, more biocompatible cancer immunotherapies that do not rely on genetically modified organisms (GMOs).
The study has been accepted for publication in the Journal for ImmunoTherapy of Cancer.
Cancer remains a leading cause of death worldwide. While revolutionary immunotherapies such as immune checkpoint inhibitors and CAR-T cell therapy have been developed, they face challenges including high costs, immune-related adverse events, limited efficacy in solid tumours, and immunosuppressive mechanisms within the tumour microenvironment.
Bacterial cancer therapy has been explored for over a century, and recent studies have revealed that certain bacterial species can selectively colonise and proliferate in the hypoxic and immunosuppressive tumour environment. However, most previous research has focused on genetically engineered Escherichia coli or Salmonella typhimurium strains, raising concerns about biosafety, complex manufacturing processes, and stringent regulatory requirements.
This study focused on naturally occurring, non-engineered marine bacteria to explore their potential for cancer therapy.
The research team evaluated the antitumour activity of multiple marine bacterial strains including P. angustum, P. phosphoreum, P. aquimaris, A. logei, and P. indicum in colorectal cancer mouse models. Only P. angustum demonstrated significant antitumor effects and prolonged survival. Other bacterial strains caused death within two days of administration due to high toxicity.
Mice treated with P. angustum showed no weight loss or haematological abnormalities. Complete blood counts, biochemical analyses, and histological examinations revealed no signs of toxicity. Inflammatory cytokine elevation was significantly lower compared to toxic strains, and bacteria were cleared from vital organs (except liver) within 24 hours.
Intravenously administered P. angustum selectively accumulated in tumour tissues with abundant colony formation. In contrast, minimal colonisation was observed in healthy organs including heart, lungs, kidneys, and spleen.
The antitumour effects of P. angustum are mediated through two mechanisms. The first is through direct tumour lysis. Natural exotoxins (including haemolysins) produced by the bacterium directly destroy cancer cells. The other mechanism is through immune system activation. This promotes intratumoral infiltration of T cells, B cells, and neutrophils, and enhances production of inflammatory cytokines such as TNF-α and IFN-γ.
When tumour-free mice were rechallenged with cancer cells 120 days after initial treatment, all mice completely rejected secondary tumour growth. This demonstrates that P. angustum therapy induces potent and durable antitumour immunological memory.
P. angustum showed significant antitumour effects not only in inflammation-driven colorectal cancer models but also in drug-resistant triple-negative breast cancer (TNBC) models. This suggests potential application beyond colorectal cancer.
The researchers said the study shows that naturally occurring, non-engineered bacteria can function as safe and effective cancer immunotherapy agents. Future research will focus on validation across various cancer types, evaluation of combination effects with immune checkpoint inhibitors, and detailed analysis of long-term immune memory.
Further elucidation of the molecular mechanisms underlying P. angustum‘s tumour-selective colonisation and immune activation will facilitate development of more effective therapeutic approaches.