Overcoming acquired treatment resistance is one of the major challenges in the fight against cancer.
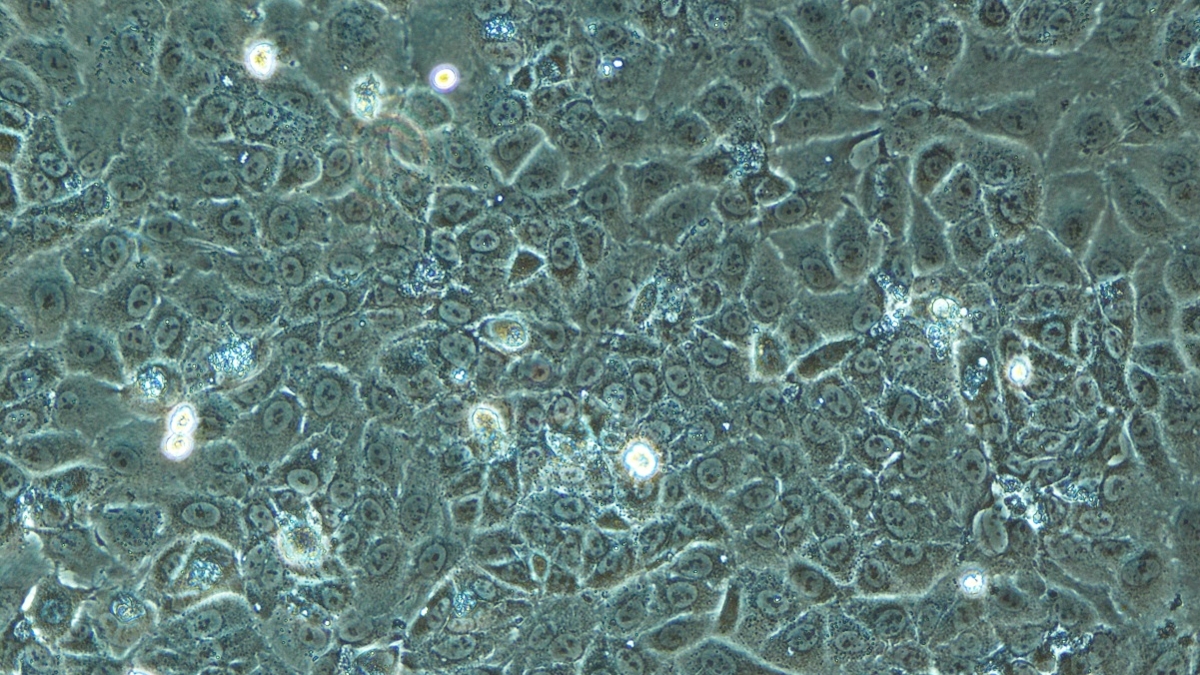
While combination therapies hold promise, their toxicity to healthy tissue remains a major hurdle. To anticipate these risks, researchers at the University of Geneva (UNIGE) in Switzerland have developed in vitro models of the kidneys, liver, and heart – three organs particularly sensitive to such therapies. This fast, animal-free approach paves the way for safer evaluation of new treatments. The findings are published in Biomedicine & Pharmacotherapy.
Recent advances in immunotherapy, targeted therapies, and gene therapies have significantly improved survival rates for patients with cancer. However, over time, many tumours develop resistance to these treatments, undermining their effectiveness. The phenomenon, known as acquired resistance, has become one of the major challenges in oncology.
To overcome this resistance, the most promising strategies involve combination therapies using multiple drugs. While these approaches enhance therapeutic effectiveness, they often cause serious toxicity in healthy organs and tissues, restricting their clinical application. To address this risk, a team at the University of Geneva (UNIGE) has developed a laboratory platform to rapidly test the toxicity of such drug combinations without animal models.
“This platform models the human kidney, heart, and liver in vitro, as clusters of cells derived from human tissue. These three organs are especially vulnerable to drug toxicity,” said Patrycja Nowak-Sliwinska, associate professor in the School of Pharmaceutical Sciences at the UNIGE Faculty of Science and member of the Centre for Translational Research in Onco-Haematology (CRTOH) at the Faculty of Medicine.
‘‘With this platform, we can study how new drug combinations interact with these organs and then decide whether it is justified to move on to in vivo testing in humans or animals.”
Using the approach, scientists from the School of Pharmaceutical Sciences, in collaboration with the UNIGE Faculty of Medicine and Geneva University Hospital (HUG), tested two specific drug combinations currently in development, C2 (erlotinib HCl, dasatinib, tubacin, tacedinaline) and REMP (erlotinib HCl, parthenolide, metformin HCl, RAPTA-C).
“We found that C2 exhibited significant liver toxicity. This indicates that proceeding to in vivo testing with this combination may not be appropriate,” the researcher said.
This method is particularly fast, as it takes only two weeks to obtain results, compared to 10 weeks or more for tests carried out using animal models.
‘‘In addition to saving a significant amount of time, this approach is fully in line with the 3R principle, which aims to ‘reduce’, ‘replace’ and ‘refine’ the use of animal models in research,’’ the scientists said.
Ultimately, the next step will be to extend the model to other organs and further customise the platform. Researchers plan to add new organs to the system and, in the longer term, to move beyond standard cell lines by using patient-derived cells. The development would allow drug combinations to be tested for toxicity in a more personalised way.