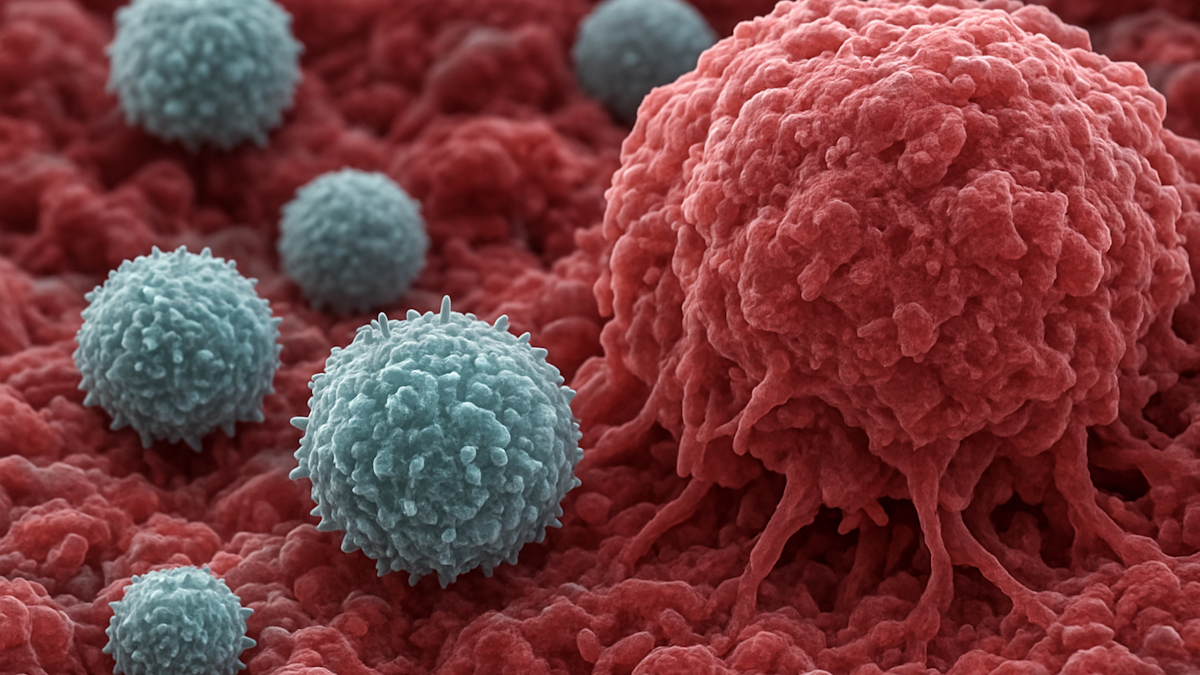
Within tumours in the human body, there are immune cells (macrophages) capable of fighting cancer, but they have been unable to perform their roles properly due to suppression by the tumour.
KAIST researchers have overcome this limitation by developing a new therapeutic approach that directly converts immune cells inside tumours into anticancer cell therapies.
KAIST has announced that a research team led by Ji-Ho Park of the Department of Bio and Brain Engineering has developed a therapy in which, when a drug is injected directly into a tumour, macrophages already present in the body absorb it, produce CAR (a cancer-recognizing device) proteins on their own, and are converted into anticancer immune cells known as “CAR-macrophages.”
Solid tumours—such as gastric, lung, and liver cancers—grow as dense masses, making it difficult for immune cells to infiltrate them or maintain their function. As a result, the effectiveness of existing immune cell therapies has been limited.
CAR-macrophages, which have recently attracted attention as a next-generation immunotherapy, have the advantage of directly engulfing cancer cells while simultaneously activating surrounding immune cells to amplify anticancer responses.
However, conventional CAR-macrophage therapies require immune cells to be extracted from a patient’s blood, followed by cell culture and genetic modification. This process is time-consuming, costly, and has limited feasibility for real-world patient applications.
To address this challenge, the research team focused on “tumour-associated macrophages” already accumulated around tumours.
They developed a strategy to directly reprogramme immune cells in the body by loading lipid nanoparticles—designed to be readily absorbed by macrophages—with both mRNA encoding cancer-recognition information and an immunostimulant that activates immune responses.
CAR-macrophages were created by “directly converting the body’s own macrophages into anticancer cell therapies inside the body.”
When this therapeutic agent was injected into tumours, macrophages rapidly absorbed it and began producing proteins that recognize cancer cells, while immune signalling was simultaneously activated. As a result, the generated “enhanced CAR-macrophages” showed markedly improved cancer cell–killing ability and activated surrounding immune cells, producing a powerful anticancer effect.
In animal models of melanoma (the most dangerous form of skin cancer), tumour growth was significantly suppressed, and the therapeutic effect was shown to have the potential to extend beyond the local tumour site to induce systemic immune responses.
Ji-Ho Park said: “This study presents a new concept of immune cell therapy that generates anticancer immune cells directly inside the patient’s body,” adding that “it is particularly meaningful in that it simultaneously overcomes the key limitations of existing CAR-macrophage therapies—delivery efficiency and the immunosuppressive tumour environment.”
The research was led by Jun-Hee Han, of the Department of Bio and Brain Engineering at KAIST as the first author, and the results were published in ACS Nano.
Jim Cornall is editor of Deeptech Digest and publisher at Ayr Coastal Media. He is an award-winning writer, editor, photographer, broadcaster, designer and author. Contact Jim here.